What is Osteoporosis?
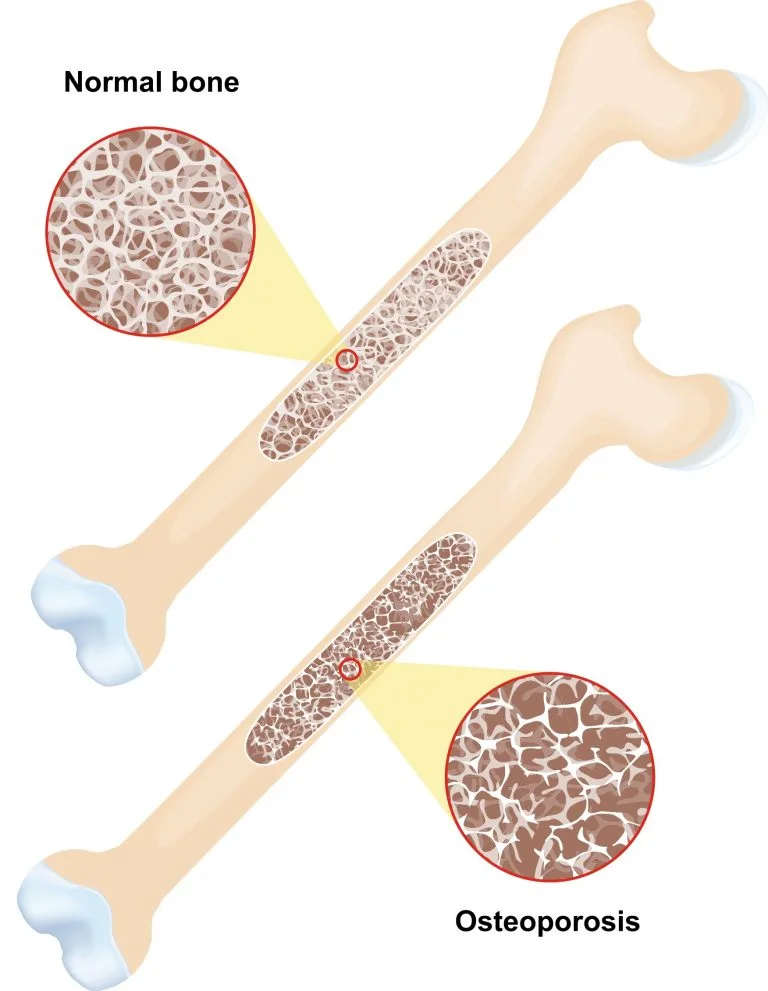
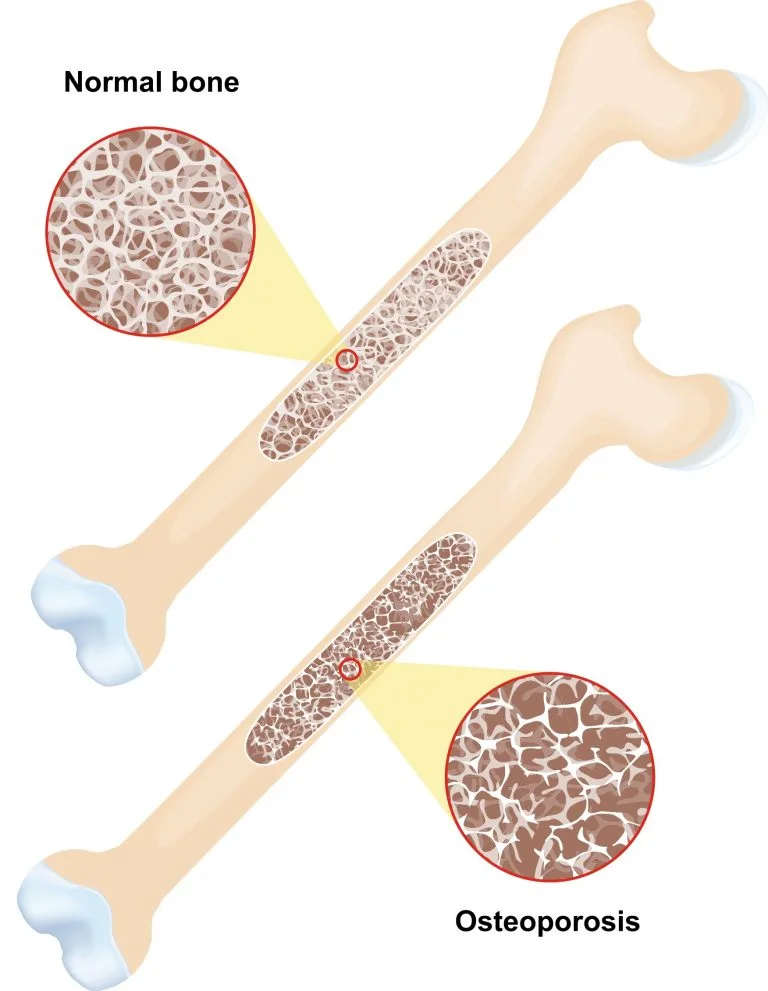
Osteoporosis is a disease that causes bones to become weak and brittle. This can be the result of the body losing too much bone, making too little bone, or both.
Strong bones are essential to your overall health because they help protect vital organs from injury, store crucial nutrients and support movement. In healthy bones, new bone tissue is created quicker than old bone tissue deteriorates, resulting in strong, dense bones that are hard to break.
According to the National Osteoporosis Foundation, “Viewed under a microscope, healthy bone looks like a honeycomb. When osteoporosis occurs, the holes and spaces in the honeycomb are much larger than in healthy bone.”
Causes of Osteoporosis
Osteoporosis has several causes and can affect people of all ages and genders. One common cause of osteoporosis is vitamin D deficiency.
Vitamin D helps the body absorb calcium, a mineral that helps build bone strength and maintain muscle function.
- Vitamin D deficiency occurs when the body is not getting enough vitamin D, either through food, dietary supplements or sunlight.
- Too little vitamin D can trigger the release of parathyroid hormone, which causes bones to release calcium constantly into the bloodstream. This can cause bones to break down and lose their density, leading to osteoporosis.
- Low amounts of vitamin D have also been associated with cancer, cognitive impairment in older adults, asthma in children and an increased risk of death from cardiovascular disease.
- The symptoms of vitamin D deficiency are usually subtle, but may include muscle weakness and bone pain.
Vitamin D deficiency is not the only cause of osteoporosis. Other causes include:
- Slow bone growth during childhood. People who start out with lower reserves of bone are more likely to develop osteoporosis later in life.
- Menopause. The reduction of estrogen production that occurs during menopause can lead to osteoporosis in older women. This decrease in estrogen speeds up the rate of bone loss, especially during the first few years after menopause.
- Some diseases and medical conditions. Alcoholism, anorexia nervosa, kidney disease, hyperthyroidism and certain gastrointestinal disorders have been linked to osteoporosis.
- Certain medications. Long-term use of certain anticonvulsants and anti-inflammatory drugs can lead to osteoporosis.
Symptoms and Risks
Osteoporosis has no symptoms until a bone breaks. However, a bone density test can help evaluate how strong your bones are and determine whether or not you have osteoporosis. A bone density test can also identify how likely you are to break a bone.
Typically, your doctor will order a bone density test if he or she feels you are likely to develop osteoporosis.
Risks for Women and Older Adults
Age and Gender both play key roles in whether someone is at risk of developing osteoporosis.
After age 30, bone deposits occur at a slower rate than bone withdrawals, leading to decreased bone density. Also, reduced calcium absorption and vitamin D deficiency are common in older adults.
Although osteoporosis can occur in men and women at any age, it is most common in older women. According to Harvard Health Publications, osteoporosis starts earlier in women and gets worse faster because of midlife hormonal shifts.
Other risk factors include:
- Weight. People who are below their recommended body weight are more likely to get osteoporosis than people who are normal weight or overweight.
- Family history. People with one or more family members with osteoporosis may have an increased risk of developing the disease.
- Ethnicity. According to the National Institute of Health, Caucasian women and Asian women are most likely to get osteoporosis.
- Smoking. There is a direct correlation between tobacco use and decreased bone density.
- Inactivity. A lack of exercise or physical activity can increase the rate of bone loss.
- Certain medical conditions. Some autoimmune disorders, gastrointestinal disorders and cancers can increase the likelihood of osteoporosis
- Some medical procedures. People who have had gastrointestinal bypass procedures may have an increased risk of developing osteoporosis.
Treatment and Prevention
The following tips can help strengthen bones and prevent fractures caused by osteoporosis.
1. Eat a Diet Rich In Calcium
A well-balanced diet is important at any age, but is especially important for people with osteoporosis.
Foods that are good sources of calcium include:
- Dairy products such as milk, cheese and yogurt
- Calcium-fortified soy milk
- Broccoli
- Tofu
- Kale
- Sardines and canned salmon
- Beans
- Almonds
Recommended Daily Calcium Intake